A Guide to Diabetes Medications for Better Blood Sugar Control
Introduction to Diabetes Medications
Diabetes is a chronic condition affecting millions worldwide, characterized by the body’s inability to regulate blood sugar levels effectively. Managing diabetes requires a multifaceted approach, including lifestyle changes, diet, and often, medication. Understanding the array of diabetes medications available is crucial for effective blood sugar control. This guide aims to provide an in-depth look at the different types of diabetes medications, their functions, and their roles in managing diabetes.
Types of Diabetes Medications
Diabetes medications can be broadly categorized into several types, each working in a unique way to help manage blood sugar levels:
- Insulin Therapy: Essential for individuals with Type 1 diabetes and some with Type 2, insulin helps regulate blood sugar by mimicking the hormone produced by the pancreas.
- Metformin: Often the first line of defense in Type 2 diabetes, it works by reducing glucose production in the liver and improving insulin sensitivity.
- Sulfonylureas: These stimulate the pancreas to release more insulin and are often used when metformin alone is insufficient.
- DPP-4 Inhibitors: These help increase insulin production and decrease glucose production in the liver, offering a balanced approach to blood sugar control.
- SGLT2 Inhibitors: By preventing glucose reabsorption in the kidneys, these medications help excrete excess glucose through urine.
Each of these medications has specific roles and potential side effects, which should be discussed with a healthcare provider to tailor the treatment to individual needs.
Insulin Therapy: A Closer Look
Insulin therapy is a cornerstone for many living with diabetes, particularly for those with Type 1 diabetes. It involves the administration of insulin through injections or an insulin pump. There are various forms of insulin, including:
- Rapid-acting insulin: Begins working within minutes and is used to control blood sugar spikes during meals.
- Short-acting insulin: Covers insulin needs for meals eaten within 30-60 minutes.
- Intermediate-acting insulin: Covers insulin needs for about half a day or overnight.
- Long-acting insulin: Provides a steady level of insulin for a full day.
The choice of insulin type depends on factors such as lifestyle, blood sugar levels, and specific health needs. Proper insulin management is vital to avoid complications such as hypoglycemia or hyperglycemia.
Oral Medications: Metformin and Beyond
For many with Type 2 diabetes, oral medications are an effective way to manage blood sugar levels. Metformin is often the first medication prescribed due to its effectiveness and safety profile. It works by reducing the amount of sugar the liver releases into the blood and improving insulin sensitivity.
Beyond metformin, other oral medications include:
- Sulfonylureas: These drugs help the pancreas produce more insulin and are often used when metformin is not enough.
- Thiazolidinediones: These improve insulin sensitivity but come with potential side effects that need consideration.
- DPP-4 Inhibitors: These medications help increase insulin production and decrease liver glucose production, offering a balanced approach to blood sugar control.
Each medication has its mechanism of action, benefits, and potential side effects, making it essential to work closely with healthcare providers to find the most suitable treatment plan.
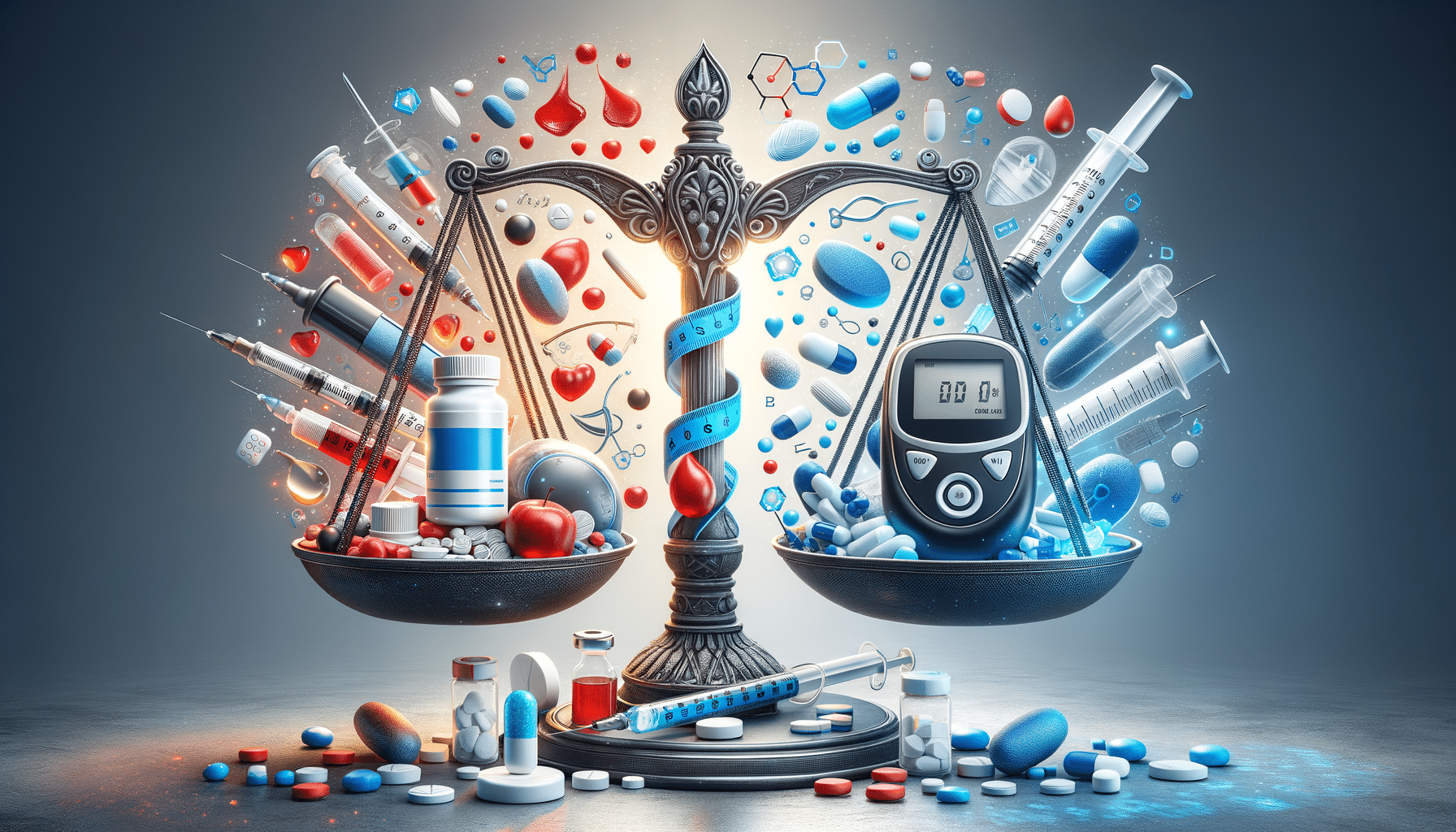
Choosing the Right Medication
Selecting the appropriate diabetes medication involves a comprehensive evaluation of individual health needs, lifestyle, and potential side effects. Factors to consider include:
- Type of diabetes: Type 1 diabetes often requires insulin therapy, while Type 2 diabetes may be managed with oral medications or a combination of treatments.
- Blood sugar levels: Consistent monitoring helps determine the effectiveness of a medication regimen.
- Lifestyle factors: Diet, exercise, and daily routines can influence medication choices and effectiveness.
- Side effects: Understanding potential side effects and how they may impact quality of life is crucial.
Ultimately, the goal is to maintain optimal blood sugar control while minimizing side effects, requiring a personalized approach and ongoing communication with healthcare providers.
Conclusion: Empowering Diabetes Management
Understanding diabetes medications is a critical component of managing the condition effectively. With a variety of options available, individuals can work with their healthcare providers to tailor a treatment plan that best suits their needs. By staying informed and proactive, those living with diabetes can maintain better control over their blood sugar levels, leading to improved health outcomes and quality of life. Regular check-ups, lifestyle adjustments, and adherence to prescribed medications form the foundation of successful diabetes management.